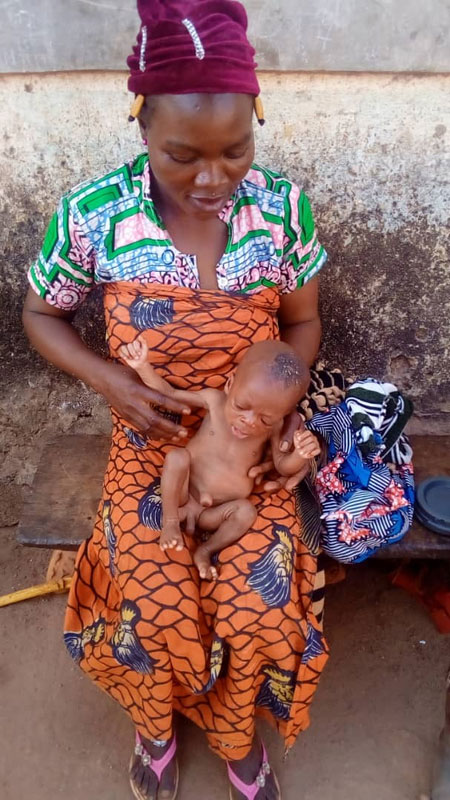
The Foundation helps children suffering from severe acute malnutrition
The social worker and Eric, the nutritionist, explain
What causes severe acute malnutrition?
Eric: “The occurrence and emergence of severe acute malnutrition can be related tosocial, religious, economic, cultural and religious issues. Indeed, the majority of the Beninese population has low purchasing power and lives in isolated areas with very poor access roads. All these factors limit availability of quality food and care. The high household size due to polygamy, multiple births, and low use of family planning methods, influences the nutritional status of children. In addition, there are several food taboos and prohibitions in Benin. In the north of Benin, the population struggles to practice exclusive breastfeeding. Some ethnic groups consider colostrum unfit for consumption. Others refuse to give meat, fish, or eggs to their children because of the risk of predisposing them to theft. In still other ethnic groups, fathers are given priority in the sharing of meals, especially with regard to eating meat.”
How is severe acute malnutrition managed?
The hospital social worker: “Acute malnutrition is treated at various levels of the health pyramid depending on the form (moderate, severe without complication or severe with complication) and following an elaborate protocol. Severe acute malnutrition with complications is treated in therapeutic nutrition centres, which are mostly located in the paediatric wards of regional and departmental hospitals, for an average of 14 days of hospitalisation.”
How is the symbiosis of the actions of the different actors involved in the care process achieved?
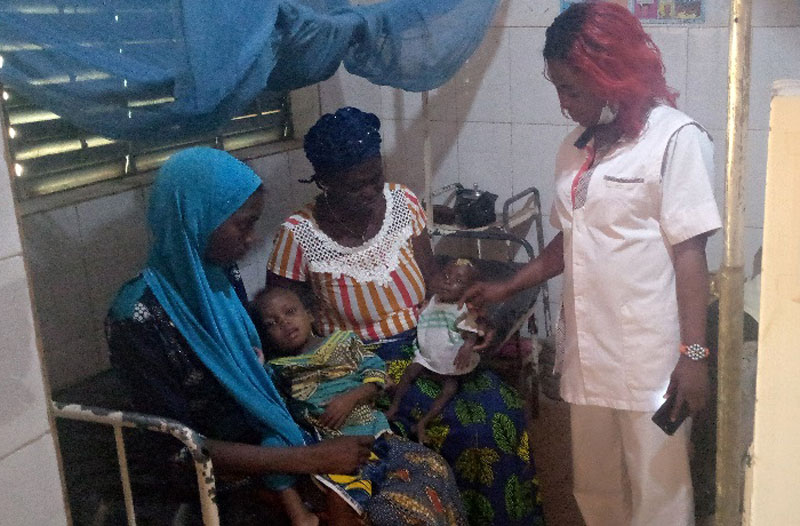
Eric: “In the municipalities where the Foundation Hubi & Vinciane operates, a dynamic team consisting of a paediatrician, nurses, care assistants, social workers and nutritionists work together on the various components of the treatment to ensure that the children are taken care of. Medication treatment is provided by the paediatrician, nurses, and care assistants. It aims to treat all diseases associated with malnutrition. Nutritional treatment and psychosocial treatment are provided by the assistant under the supervision of the paediatrician. Indeed, an assistant is a paramedic who takes care of social cases.”
What is the role of a social worker in the care of a malnourished child?

The social worker: “As part of the management of severe acute malnutrition with complications, I welcome the mothers of malnourished children or the nurses to settle them. I register the children and take anthropometric and clinical parameters to establish a file for each patient. I educate the mothers or carers on the procedures to follow during treatment. I prepare the therapeutic milks (F75 or F100), elaborate the daily food ration for each child, the distribution of meals and the follow-up of the administration of the meals to the children.”
What is the role of the nutritionist in the management of a malnourished child?
Eric: “I act as a liaison between the hospital and the community. I screen cases in the community and refer them to the hospital’s paediatric department. I am the direct link with the social worker for a good follow-up of malnourished children discharged from the hospital. I organise home visits to the parents of malnourished children. During these visits, I educate the parents on healthy and balanced nutrition and many other topics to prevent a probable relapse. I also provide cooking demonstrations to show balanced recipes adapted to ensure the good nutritional status of children recovered from malnutrition.”
What does the mother or carer do with the child?
The social worker: “During this 14-day period, the mother or guardian of the child receives training on balanced nutrition and the preparation of various fortified porridges. She is also made aware of food and body hygiene. This training enables her to better care for the child at home after the hospital treatment. It should be noted that it is not always easy to refer a malnourished child detected in the community.”
What are the difficulties encountered?
The most affected areas are often inaccessible. Mothers of children find it difficult to leave home to come and do the 14 days of treatment at the risk of losing their husbands or remaining children. We also have a very low standard of living which does not allow the mother to easily last the 14 days because the child is taken care of but not the mother. We also note the low level of involvement of the husbands. However, we would like to thank the Hubi & Vinciane Foundation, which fights every moment to save the children we refer.”